Day 2 :
Keynote Forum
Tanju Surmeli
President of International Board of Quantitative Electrophysiology, USA
Keynote: Evidence supporting neurofeedback for adult psychiatric disorders.
Time : 09:40-10:25

Biography:
Tanju Sürmeli received his Medical Doctor degree from Dokuz Eylül University in 1984 in Ä°zmir, Turkey. He did his residency training in Psychiatry and Neurology at University of Connecticut/Institute of Living, Yale, and University of Texas, San Antonio. He is a board and ECFM certified psychiatrist. He had completed Harvard Medical School’s Global Clinical Scholars Research Training Program and a Research Fellowship in EEG and psychopharmacology at New York Medical College.
Abstract:
Psychiatric disorders interfere with daily-life activities and treated with psychological and pharmacological treatments. Psychopharmacology and Psychotherapy for their high rates of failure to meaningfully improve outcomes, saying it's time to figure out how to develop "the next generation of interventions." A new route map has been drawn for the diagnosis and treatment of psychiatric diseases. The National Institute of Mental Health (NIMH)'s call for a more rigorous and evidence-driven approach to mental healthcare. It is time that psychiatry moves away from its present focus on medications and takes a new direction that uses other modalities of care evidence-based psychotherapies. Psychiatry and Psychology are the only specialty that doesn't actually look at the organ it treats. Patients deserves more better. We need to devote our self to efficient evidence based diagnosis of disorders and personalized treatments. New methods of treatment are necessary and Neurofeedback (NF) is one treatment that seems to be effective in psychiatric disorders. I am going to talk about evidence supporting neurofeedback for adult psychiatric disorders
Keynote Forum
Caron Leid
Alzheimer Advocate & Care Giver Expert, USA
Keynote: Alzheimer’s-living with the disease
Time : 10:25-11:10

Biography:
Caron Leid is an author, Alzheimer’s advocate , keynote speaker and caregiver, Caron is a doctoral candidate and has published several articles on the topic of living with Alzheimer’s disease. Caron Leid is a dedicated mother and passionate student. Her book Alzheimer’s: What They Forget To Tell You has been featured on Chapters, Amazon, Barnes & Noble and international bookstores. Her career and passion surrounds educating others and she believes in the pay it forward principle. As the primary caregiver for her mother for the last 17 years, Caron hopes that her story can inspire people that struggle with Alzheimer’s disease and the various aspects surrounding the disease.
Abstract:
When my mother was first diagnosed 17 years ago, at the age of 57, I had a newborn and was propelled immediately into the sandwich generation. There was few resources or information surrounding living with the disease in the year 2000. I started journaling my experience more for cathartic purposes, and then had the courage enough to publish it in hopes of helping others.
Since then, I have written several journal articles on the topic of Alzheimer’s disease and living with the disease. I have appeared on CTV National News, I have worked with the Alzheimer’s Society of Canada, and have spoken at an International Alzheimer Disease and Dementia Conference in 2015. 17 years of the day to day emotional, mental, and physical management of the disease has provided me a unique perspective and the ability to help educate others. I am presently working on my second book on the disease and revising my first book to include the palliative care experience. I have seen this disease from the beginning and now I am witnessing the end stages first hand. My mother still resides with me, as we journey toward the end of this disease. I am now an expert in living with the disease as a sandwich generation primary caregiver. I have gone through the disease and all the collateral damage that takes place alongside of it, including compassion fatigue. Since my mother’s diagnosis 17 years ago of “Atypical” Alzheimer’s disease, and the fact that she has been in palliative care for 2 years in my home, allows me to research the disease first hand, and show the world that caregiving is an integral part of managing and living with Alzheimer’s disease.
- Psychiatric Nursing | Neuro Cognitive Disorder | Couple Therapy for Psychological Disorders | Psychotherapy | Psychology Dialectical Behavior Therapy | Behavioral Therapy | Cognitive Behavioral Therapy | Emotion Regulation Therapy

Chair
Annamarie Paulsen
Rockdale Psychiatric Associates, USA

Co-Chair
Kelli Bridgman
Rockdale Psychiatric Associates, USA
Session Introduction
Tanju Surmeli
International Board of Quantitative Electrophysiology, USA
Title: Use of clinical electrophysiology as a biomarker diagnostic and treatment in psychiatric setting

Biography:
Tanju Sürmeli received his Medical Doctor degree from Dokuz Eylül University in 1984 in Ä°zmir, Turkey. He did his residency training in Psychiatry and Neurology at University of Connecticut/Institute of Living, Yale, and University of Texas, San Antonio. He is a board and ECFM certified psychiatrist. He had completed Harvard Medical School’s Global Clinical Scholars Research Training Program and a Research Fellowship in EEG and psychopharmacology at New York Medical College. As well as having numerous memberships (AMA, APA , AAPB, ISNR, SAN, BFE, ECNS) and and teaching positions in international medical societies’ workshops. He is also a reviewer for the Journal of Clinical EEG and Neurosciences, Psychiatry Research, Behavioural Neurology, Schizophrenia Research, and Journal of Child Psychology and Psychiatry, Neuro Biobehavioral reviews, Nature Scientific Reports and Journal of Child Psychology and Psychiatry. In 2015, upon request of the Swedish Science Academy Institution, he reviewed scientist's "Neurofeedback in Schizophrenia" placebo controlled study's grant application as an expert reviewer. In 2017, upon request of the Swedish Science Academy Institution, he reviewed scientist's "Neurofeedback in Bipolar Disorder and Borderline Disorder" placebo controlled study's grant application as an expert reviewer. In 2018, upon request of the Swedish Science Academy Institution, he reviewed scientist's "Neurofeedback in residual symptoms of Bipolar Disorder " placebo controlled study's grant application as an expert reviewer. His Schizophrenia Case Study paper was awarded in 2013, The Foundation for Neurofeedback and Applied Neuroscience (FNAN) award given to the publication that, “in its consideration, has most significantly advanced the field of neurofeedback during the preceding year”
Abstract:
Psychiatric disorders interfere with daily-life activities and treated with psychological and pharmacological treatments. For Psychopharmacology and Psychotherapy to meaningfully improve outcomes, it's time to figure out how to develop "the next generation of interventions.” A new route map has been drawn for the diagnosis and treatment of psychiatric diseases. The National Institute of Mental Health (NIMH) has called for a more rigorous and evidence-driven approach to mental healthcare. It is time that psychiatry and psychology moves away from its present focus on diagnosing subjectively and takes a new direction that uses other modalities of care; evidence-based diagnosis and treatments. Psychiatry and psychology are the only specialty that doesn't actually look at the organ it treats. Patients deserves better. We need to devote our selves to efficient evidence-based diagnosis of disorders and personalized treatments. Implementing biological markers for psychiatric disorders into laboratory-based electrophysiological diagnostic tests can significantly improve diagnosis and management of these disorders. Diagnostic electrophysiological techniques are non-invasive and relatively inexpensive. Psychiatric electrophysiology currently under utilizes such methods and plays a limited role in the diagnosis and treatment in psychiatric disorders. This status is not supported by the existing literature. I am going to talk about evidence supporting diagnostic electrophysiological biomarkers and their effectiveness in the treatment of psychiatric disorders.
Natasha Lyons
Central and North West London NHSFoundation Trust, UK
Title: Carer’s illness beliefs after first episode psychosis: Prevalence, intensity, predictors and factor structure
Time : 12:35-13:05

Biography:
Natasha Lyons is a Life Sciences graduate with a First Class Degree from University College London who recently converted to the field of Psychology (MSc). She is currently a Research Worker for the U.K. National Health Service, working on projects in collaboration with University College London, and Institute of Psychiatry, Psychology and Neuroscience, London UK. Her work encompasses first episode psychosis carers psychological experiences and psychoeducation, and the cognitive neuroscience of auditory hallucinations. Natasha is currently on the Advisory Committee for the British Psychological Society’s forthcoming National Guidelines for Family Intervention in Psychosis, writing a chapter addressing working with Diversity.
Abstract:
Objectives: To illuminate the prevalence, intensity and demographic and clinical predictors, also the factor structure, of carers key illness beliefs, after first episode psychosis (FEP).
Background and aims: Carers key beliefs about psychosis influence their emotional, behavioural and psychiatric status, as well as the healthiness of their relationship with the patient for which they care. However, little is known about the prevalence, predictors or factor-structure of these beliefs after a FEP, so we aimed to analyse this in the world's biggest sample.
Materials and methods: 254 carers of patients with FEP of extremely diverse ethnicities and cultural backgrounds were included in this study based on data from routine Carers Assessments in a London, United Kingdom, Early Intervention in Psychosis service. Twelve key illness beliefs (IPQ-Relatives; Lobban, Barrowclough & Jones, 2005) were statistically tested with 30 sample characteristic variables. Beliefs' prevalence and intensity were described. Inferential statistical analyses comprised univariate and multiple linear regressions to identify predictors independently associated with illness beliefs. Then a principal component analysis with varimaxrotation identified the factor structure.
Results: At FEP key illness beliefs were common and held with moderate intensity. 17 sociodemographic and clinical factors predicted carers’ beliefs (p < 0.05). Principal component analysis yielded three novel factors with eigen values greater than 1, accounting for 63.5% of total variance.
Conclusions: Our results have theoretical implications for the content and organisation of cognitive models of caregiving at FEP. Clinical implications relate to identifying which carers and which key illness beliefs to prioritise for early intervention.
Mariam Sedney
Secretary of the sub Council of Ministers, Suriname
Title: Psychology in Suriname: An overview of the mental health care in Suriname
Time : 14:05-14:35

Biography:
Mariam Sedney is a 28 year old young woman who is born and raised in Suriname. She has studied Psychology at the Anton De Kom University of Suriname (2011-2014) in cooperation with the Erasmus University Rotterdam, Netherlands and obtained a Bachelor of Science degree in Psychology. She worked for two years during her studies and for three years after graduation at the MoleMann Mental Health Clinics Netherlands, department Suriname. Apart from clinical based treatments, she also performed IQ tests for children in order of the Government, Assessments for companies, Progressive relaxation therapy to employees of various companies and trauma treatment to children and youth of the NosKasita Orphanage in Suriname. During this period she also attended several Psychological Symposia and trainings of the CANPA and IASP organizations mostly regarding depression and suicide. Afterwards, she worked for a year as a counselor at Creditsafe Netherlands, department Suriname, an insurance company. At the moment she is working at the Government of Suriname at the Cabinet of the Vice President as secretary of the sub council of Ministers of the Social Security system regarding health care policy.
Abstract:
Suriname is delighted to participate in this International Conference for Psychology 2018 in Paris. We aim to give a glimpse of our country and culture from a Psychological perspective. We hope that after this presentation this global platform will have an understanding of the Mental Health Care in Suriname. In this presentation the emphasis will be on the most common mental health disorders that Surinamese citizens struggle with and the connection with environmental and cultural factors. Are there additional differences in the vulnerability and etiology of the disorders in Suriname due to cultural factors? In cooperation with the Minister of Health, Suriname Psychiatric Hospital, Mental Health Clinics (e.g Mole Mann Mental Health Clinic Netherlands, department Suriname) and the University, statistics will be presented about the estimated amount of mental health patients and the most common disorders in our country. There will be an overview about the discrepancy of supply and demand regarding mental health care. Is there access for every Surinamese citizen towards Psychological treatment? Is the demand for mental health care in Suriname more than estimated, because of the taboo and stereotypical culture? How can we break through this taboo culture and bring more mental health awareness and Psychological education to family, friends and acquaintances. We will also touch upon several suicide cases in Suriname and the relation with depression. Furthermore, some insights of the most common therapy forms at the Psychiatric Hospital and mental health clinics in Suriname will be presented, along with the statistics of the Global Assessment of Functioning at the end of several treatments.
Sonja Skocic
The Melbourne Clinic, Australia
Title: Therapist drift and clinicians experiences of working with people who have eating disorders
Time : 14:35-15:05

Biography:
Sonja Skocic, PhD has extensive experience working in the field of eating disorders across various public and private settings in Melbourne Australia. She is currently the Chief Psychologist at Australia’s largest private psychiatric hospital The Melbourne Clinic, providing direction and support for staff and leads a team of over 30 registered psychologists, psychology registrars, and postgraduate students. Aside from clinical work and supervision, Sonja coordinates training and professional development for Allied Health across the hospital. Sonja is also directly involved in the development and quality improvement of educational and therapeutic programs for patients, students and staff across the hospital.
Abstract:
Several studies have suggested that clinicians are reluctant to commit to evidence-based treatment protocols (e.g., Simmons et al., 2008). The aim of this study was to explore the relationship between interpersonal experiences of working therapeutically with people that have eating disorders and therapist drift away from using evidence based treatment. Cross-sectional information was obtained from clinicians who treat eating disorders (N=165) via an online survey that included questions regarding countertransference, attitudes to evidence based protocols, and the personal experience of working therapeutically (including emotional avoidance, accommodating and enabling behaviours and rigid therapeutic interactions). Clinicians were also asked to record whether they had a lived experience of an eating disorder themselves. The results supported existing theories that describe therapist drift away from using evidence-based treatments (i.e., Waller, 2009) and highlight the impact that interpersonal factors between clinician and patient have on treatment selection and adherence to protocol. Moreover, the results suggest that problematic interpersonal factors between clinician and patient may be contributing to accommodating and enabling the eating disorder (as per Schmidt & Treasure, 2006; Treasure, 2011).
Liezille Jacobs
Rhodes University, South Africa
Title: Pregnancy Police: The (De)Criminalisation of alcohol exposed pregnancies in South Africa
Time : 15:05-15:35

Biography:
Liezille has completed her Master’s in Psychology Internship at the Center for Drug Abuse Research in Washington, DC, USA. She graduated with her PhD from Stellenbosch University, in South Africa and postdoctoral studies from Antwerp University Department of Social Medicine and Epidemiology, in Belgium. She is a Senior Lecturer at Rhodes University, South Africa. She has published more than 20 papers in reputed journals, book chapters, monographs and several blog posts on the Mail & Guardian’s Thought Leader.
Abstract:
Public discourses and policies concerning pregnant women who drink alcohol are condemnatory, blaming, and unsympathetic. Therefore, women often deny the claim that they are alcohol dependent because of the intense fear of being stigmatised. Also, the harmful effects of alcohol during pregnancy have been well documented. So, it begs the question: should women be punished or banned from drinking during pregnancy for the sake of preventing fetal harm? The purpose of this paper is to consider the appropriateness of criminalizing drinking as a means to prevent fetal harm and consequently Fetal Alcohol Spectrum Disorder (FASD). This paper presents arguments for and against the criminalisation of alcohol exposed pregnancies in order to critically analyse health policy that focuses on maternal actions only when paternal actions can be equally harmful especially when the policy is not evidenced based and when the health problem is not an individual but a systemic one. This theoretical paper critically reviewed the literature through a feminist psychology lens and evaluated whether health policy should be in faviour of criminalising pregnant women who drink or not. The search terms, ‘criminalising pregnant wom(a)en*’, ‘pregnancy police’ was used to identify articles relating to policy on pregnant women who drink. The search strategy was applied to PsycINFO, MEDLINE, Web of Science and the Global Health Database. Time restrictions were excluded to maximise the identification of relevant literature. The findings suggest that an ethically befitting and useful reaction to FASD prevention necessitates a systematic multifaceted approach that does not punish, but instead aims to assist women and children.
Abdulhameed Abdullah Bokhari
King Saud Bin Abdulaziz University for Health Sciences, KSA
Title: The association between tobacco smoking and stress, anxiety and depression among medical students at King Saud Bin Abdulaziz University for Health Sciences (KSAU-HS), Jeddah Saudi Arabia

Biography:
Abdulhameed Abdullah Bokhari is a medical student at King Saud bin Abdulaziz University for Health Sciences, Saudi Arabia, Jeddah. He attended many courses and conferences in the medical field. He is interested in doing research and voluntary work.
Abstract:
Medical school is known as being stressful, difficult to learn and may significantly affect students’ psychological well-being. Also relieving stress is one of the main reasons for smoking among college students. Our aim in this study is to assess the association between tobacco smoking and stress, anxiety and depression among medical students of KSAU-HS, Jeddah. Data were collected through a validated questionnaire to assess stress, anxiety and depression and smoking status of cigarettes, e-cigarettes, shisha and hookah among medical students. 307 medical students responded to the questionnaire from the second to the sixth year of medical school. The prevalence of smoking was as follows: 52 students (17.2%) are cigarette smokers, 21 students (7%) are e-cigarette smokers, 58 students (19.2%) are hookah smokers and 21 students (7%) are shisha smokers. Also, our study found a difference in smoking patterns between male and female students. Males have more tendencies to smoke cigarettes and hookah with a p-value of 0.01 and 0.02, respectively. Our study demonstrated that there were high levels of stress, anxiety and depression. 48% of students had stress, 54.6% of students had anxiety and 54.3% of students had some degree of depression. Female students have significantly more stress than males with a p-value of 0.003. Male gender and cigarette smokers are associated with a decreased rate of depression with a p-value of 0.035 and 0.03, respectively. We recommend that medical students need workshops on how to develop better coping skills. Furthermore, they need more counselling about smoke cessation.
A Vishal
Nizamabad Medical College, India
Title: A study of state and trait anxiety in Medical College students

Biography:
Dr A Vishal has completed his MD psychiatry at the age of 32 years from NTR university of health sciences Vijayawada. Now working as assistant professor of psychiatry at government medical college Nizamabad ,Telangana, India.
Abstract:
Back ground and Aim: Comparing to general population medical college students are showing higher levels of anxiety. So, this study was conducted to evaluate State and Trait anxiety in medical college students and its association with sociodemographic variables and institutional factors like year of education.
Materials and Methods: A cross-sectional study with a random sample of (n=210) medical college students at government medical college, Nizamabad was performed. State Trait Anxiety Inventory (STAI) was used to measure anxiety symptoms and its association with sociodemographic and institutional factors. Modified Kuppuswamy Scale was used to measure socioeconomic status.
Results: Medical students having anxiety symptoms on STAI- State anxiety 10% low severity, 64.3% medium and 25.7% high severity. STAI- Trait anxiety scores were 9% low, 58.6% medium and 32.4% high scores. 60% of the sample belongs to sub urban area which is statistically significant (P value <0.0001) and majority were first year medical students (42.9%) which is also statistically significant (P value <0.0001). Year of education showing significant levels of trait anxiety symptoms among medical college students (p value 0.020*).
Conclusion: Medical college students are having medium levels of anxiety symptoms,male gender having increased levels of anxiety symptoms comparing to females. First year medical students having increase in State anxiety symptoms and Second year medical students having high Trait anxiety symptoms.
Keywords: Medical student, state anxiety, trait anxiety

Biography:
Concepción López-Soler is a Doctor in Psychology and Specialist in Clinical Psychology. She works as Associate Professor at the University of Murcia, linked to the Virgen de la Arrixaca University Hospital Clinic for Pediatric Service. She handles a professional team with great experience training psychological treatments in childhood and adolescence.
Abstract:
Cognitive behavioral therapy (CBT) and focused trauma-CBT (Cohen, Mannarino, and Deblinger, 2006) are well-established effective treatments of child trauma effect (Saunders, Berliner, and Hanson, 2004; Arellano, Ko, Danielson, and Sprague, 2008; NCTSN, 2005; SAMHSA, 2008). Our purpose of this study was to provide empirical evidence of three treatment protocols based on CBT. One of them on Emotions Focused (EF-PEDIMET); and two others, based on the TF-CBT model (Cohen, Deblinger and Mannarino, 2006), complete (FT-PEDIMET) and brief version B-FT-PEDIMET). All treatments include virtual reality. The final sample consisted of 46 children aged between 6 and 16 years (52.2% children and 47.8% girls). The CDI (Children's Depression Inventory; Kovacs, 1992) was used to evaluate depressive symptoms (total depression, dysphoria and self-esteem). The efficacy was analyzed using Student's t-test and the effect size index of the standardized mean difference (d). The results showed statistically significant differences and large effect sizes in the three treatment conditions for reduction of total depression; FT-PEMIDET (p.04, d.79), B-FT-PEDIMET (p.001, d.1.26) and EF-PEDIMET (p.002, d.1.32). The dysphoric symptoms improved significantly with all three models; FT-PEMIDET (p.017, d.73), B-FT-PEDIMET (p.005, d.1.01) and EF-PEDIMET (p.016, d.78). Self-esteem, as expected, improved significantly with both CBT-FT-based models- FT-PEMIDET (p.001, d.1.14), and B-FT-PEDIMET (p.006, d.99).
Sasha A Hurst (Poster-2)
University of Pretoria, South Africa
Title: A Review of the provision of mental healthcare services for elderly patients in Tshwane District, Gauteng Province in South Africa
Biography:
Sasha Hurst is a fourth-year medical student at the University of Pretoria in South Africa. She has had a passion for medical research from a young age and is particularly interested in research influencing policy and improving healthcare outcomes. She started her research journey in 2016 by assessing the provision of mental healthcare services in Tshwane District, Gauteng Province. That year, she made suggestions to the Office of Health Standards Compliance, contributing to the development of their hospital assessment tool. In addition, she is currently one of the facilitators at the Tuks Undergraduate Research Forum at the Faculty of Health Sciences, University of Pretoria.
Abstract:
Statement of the Problem: According to the WHO, an elderly individual is defined as anyone who is 60 years of age or older.1The global elderly population is projected to almost double its size by 2050.1Compared to other African countries, South Africa has relatively well-resourced mental health services.2However, most patients with a mental illness – including the elderly- do not get the required healthcare.3Healthcare facilities in Tshwane District, Gauteng province that provide a mental healthcare service for elderly patients are scarce and insufficient information exists on their quality. The aim of this study is to describe the provision of mental healthcare services for elderly patients in Tshwane District.
Methodology & Theoretical Orientation: An observational cross-sectional study design was used. The study setting included all public sector hospitals, clinics, community health centres (CHC) and non- governmental organizations (NGO) that provide these services. A validated checklist of 39 items assessed their quality, generating a score. Key informants were interviewed using semi-structured questions. Interviews were audiotaped and all results captured into Microsoft Excel. Thematic analysis was conducted.
Findings: 64 facilities were invited to participate. Of these facilities, 27 (42.2%) were assessed. CHCs had the highest mean score for service provision due to recent renovations while NGOs had the lowest scores. The main shortcomings were: inadequate infrastructure, poor lighting and lack of adequate wheelchair access. There was also a shortage of health professionals for this population. Key informants verified these difficulties with amongst others, the lack of medications on the essential drug list and inadequate implementation of the Mental Healthcare and Older Person’s Acts.
Conclusion & Significance: There is a shortage of specialized, quality services for this vulnerable growing population. To avoid future tragedies where patients with mental health illnesses have died (“Life Esidimeni”), increased surveillance of all facilities tasked with providing such services is mandatory.
Valentina Asabella (Poster-3)
Community Mental Health Center, Albania
Title: Alteration of biochemical parameters in prolonged antipsychotics and antidepressive therapy

Biography:
Valentina Asabella is a Doctor in Regional Health Authority, Tirana, Albania. Her research interests are Psychiatry, Psychology & Mental Health.
Abstract:
Introduction: Psychopharmacology has become more complex over the past decade or so, with many more medications available from different pharmacologic classes.
Aim: The aim of the study was to investigate the alterations of biochemical parameters in patients with schizophrenia and bipolar disorders treated with atypical antipsychotic and antidepressant drugs (olanzapin, risperidon, clozapin, tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs).
Material & Methods: Fifty three patients in prolonged treatment with schizophrenia and bipolar disorders were evaluated; 16 women and 37 men aged between 18 and 75 years. Blood collection and examination were performed at our laboratory with autoanalyzer or SAT 450 and MAGLUM 900.
Results: Evaluation after repeated measurements indicated significant differences in comparing the mean values obtained in each patient. The indicators of development of metabolic syndrome showed a significant increase of lipid panel especially triglycerides, total cholesterol, fasting glucose, CK level and hepatic enzymes (p<0.01). Plasma level of prolactin was significantly higher in patients with the predominant negative symptoms of schizophrenia 4.88 (±3.72).
Conclusion: This study supports the hypothesis that changes in the studied parameters are associated with the treatment with atypical antipsychotic and antidepressant drugs. Monitoring patients' blood compositions could result in better prognostic evaluations and aid in determining additional systemic treatment options.
Xin Ma (Poster-4)
Beijing Anding Hospital, Republic of China
Title: Development and psychometric analysis of mental health scale for Beijing residents

Biography:
Xin Ma has completed her BSM degree in 1983 from Peking University Health Science Center and went to Western State Hospital in Washington to study Geriatrics and Community Psychiatry in 1996. She is a Professor and a Doctoral Supervisor at Beijing Anding Hospital, Director of Beijing Mental Health Institute and Director of China Mental Health Association. She has published more than 30 papers in reputed journals.
Abstract:
The study aims to develop a new Mental Health Scale for residents over 18 years old and under age 65 in Beijing. It contains three stages: Firstly, based on the Beijing residents’ mental health evaluation system and the characteristics of Beijing residents, organizing and writing entries through the round of expert evaluation method to determine the first edition of the scale. Secondly, using stratified random sampling method to extract 850 Beijing residents. Using item analysis and exploratory factor analysis to analyze the sample data, and forming the draft of the second edition. Thirdly, using multistage stratified random sampling to select 700 residents to send out scale. And collecting 110 patients’ answer of the scale to test reliability and validity of scale. This scale including six first-level dimensions of 80 entries. The Cronbach's a coefficient of the total scale is 0.969.The Pearson correlation coefficient between the secondary dimension and the first order dimension is between 0.579-0.746, P<0.01. The correlation coefficient between the dimensions and the total scale was between 0.792 and 0.891 (P≤0.01). The scores of the patients were compared with the residents in the total scale T = 9.750. The questionnaires TCSQ, PANAS, SQ, EPQ were used as the calibration questionnaire. The scores of these scales were significantly correlated with the dimensions of the same content measured in the Beijing Mental Health Scale. It was indicating that there’s a good reliability and standard validity, which can be used as an effective assessment tool of Beijing residents mental health.
Concepción López-Soler (Poster-5)
University of Murcia, Spain
Title: Comorbidity or complex PTSD? A study in children exposed to IPV

Biography:
Concepción López-Soler is a Doctor in Psychology and Specialist in Clinical Psychology. She works as an Associate Professor at the University of Murcia, linked to the Virgen de la Arrixaca University Hospital Clinic for Pediatric Service. She handles a professional team with great experience training psychological treatments in childhood and adolescence.
Abstract:
Statement of the Problem: There are few empirical studies that document the comorbidity between PTSD and other psychopathological alterations in minors exposed to interpersonal partner violence (IPV). We believe that it is necessary to carry out, from a clinical and treatment point of view, the diagnosis of complex PTSD, instead of assigning the diagnosis of PTSD associated with other disorders (DSM-5, 2013). This is the question that is currently being debated. The purpose of this study was to determine the comorbidity between PTSD and general psychopathology in children exposed to IPV.
Methodology: A total of 153 children exposed to intimate partner violence took part, who had severe psychological disturbances [76 children (49.7%) and 77 girls (50.3%), aged between 8 and 17 years; (M=11.50; Ds=2.72),]. The instrument of measurement was CBCL/6-18 (Achenbach and Rescorla, 2001), which evaluates behavioral and emotional problems; and Child Post-Traumatic Stress Disorder Symptom Scale (CPSS; Foa, Johnson, Feeny and Tredwell, 2001) consisting of 17 symptoms.
Findings: Fifty-nine percent of the children presented three or more empirical syndromes of the CBCL and severe symptoms of PTSD. It was also found that, with greater depressive/anxious symptomatology, somatic complaints and internalizing symptoms, the PTSD symptoms increased.
Conclusion & Significance: The results are similar to those found in other studies like Cloitre et al., 2009, Fan et al., 2011, Hodges et al., 2013, Jonkman et al., 2013, Margolin and Vickerman, 2011, Scheeringa, 2015, which makes us think not only about the difficulty of the diagnosis when the symptoms become more complex, but the practical implications that are derived for a more effective treatment.
- Psychiatry | Psychology | Psychology Health | Neuroscience | Child Psychology | Mental Health | Behavioral Psychology | Positive Psychology/Science of Happiness | Women Mental Health | Child & Adolescence Behavioral Therapy

Chair
Neeta Sinha
Pandit Deendayal Petroleum University, India

Co-Chair
A Vishal
Nizamabad Medical College, India
Session Introduction
Annamarie Paulsen
Rockdale Psychiatric Associates, USA
Title: Successful outpatient treatment of opiate addiction
Time : 11:20-12:20

Biography:
Annamarie Paulsen is a Board Certified Child, Adolescent and Adult Psychiatrist and Former Nurse with over 35 years working in a multidisciplinary psychiatric setting in the US. She is a Medical Director in Rockdale Psychiatric Associates Conyers, Georgia USA. She has completed her Bachelor of Nursing in Medical College of Georgia. In Emory University, she has completed her Master’s in Nursing. In University of Iowa, she accomplished her Master’s in Preventive Medicine and Psychiatric Epidemiology. She has completed her Doctor of Medicine in Morehouse School of Medicine.
Abstract:
Looking forward to our "Sublocade Launch” AND looking back on over five years of outpatient treatment of opiate addiction in a suburban private USA psychiatric practice using Suboxone or generic buprenorphine
The presenters will give a detailed description of their experience using buprenorphine and naltrexone combination medications to treat opiate addiction. We will cover our successes and our struggles to treat clients who are opiate-dependent highlighting best practice methodologies.
The attendees will be "brought into our clinic" to better understand how to liaison with therapists, community resources and and family and friends. We will describe in detail our treatment protocol and our emphasis on 12- step principles and therapy techniques including DBT and Emotional Freedom Tapping. We will give real-life examples of these treatment modalities reinforce a growing sense of self-love, compassion and self- forgiveness. We will also review the use of these medications in clients with medical conditions and at varying stages of life.
We will also highlight our early clinical experience with Sublocade, the new monthly injection form of buprenorphine. This new delivery system will eliminate some of the difficulties associated with the prescription of oral agents. We will present the management of our clients using this new delivery system.
Harry G. Segal
Cornell University & Weill Cornell Medical School, USA
Title: The Search for the self in the age of the brain
Time : 12:25-12:55

Biography:
Harry Segal graduated with a BA and MA in English Literature from Columbia (1990); He received a Ph.D. in English Literature Yale University and second doctorate in Clinical Psychology from the University of Michigan in 1990. He completed a post-doctoral fellowship in the Department of Psychiatry, University of Michigan Medical School, and joined the faculty at Cornell in 1998. His work has focused on the clinical assessment of narrative and, more recently, models of the self. His publications include empirical studies on adolescent suicidality and depression, borderline personality disorder, and theoretical work on the creative process in fiction.
Abstract:
Although the assertion that we all have “self” may seem indisputable, ideas about what the self is have actually evolved and changed radically since the middle ages when the words self and spirit were interchangeable. In this paper, I track the various versions of the self since Descartes’ attempt to bridge the anatonomical and the religious, touching on psychoanalytic approaches and more recent cognitive models. All of these, as useful as they are, are shorthand explanations for self experience; and yet there is no part of the brain where you can find the “self.” Instead, there are neurological pathways connecting perception, memory and imagination. Consciousness is whatever we’re associating to at the moment, and self experience is just one class of those associations. The experience of having a self is actually the continuity of a brain associating to experience and relating those new experiences to memory. Considered in this light, it’s not I think therefore I am, it’s I associate therefore I am. This associative model of consciousness can be used to explain social-constructivist and interpersonal models of the self, as well as new ways of understanding identity, psychopathology, and creativity.
Sonja Skocic
The Melbourne Clinic, Australia
Title: Recovering from an eating disorder in a Western World
Time : 13:55-14:25

Biography:
Sonja Skocic, PhD has extensive experience working in the field of eating disorders across various public and private settings in Melbourne Australia. She is currently the Chief Psychologist at Australia’s largest private psychiatric hospital The Melbourne Clinic, providing direction and support for staff and leads a team of over 30 registered psychologists, psychology registrars, and postgraduate students. Aside from clinical work and supervision, Sonja coordinates professional development and quality improvement of educational and therapeutic programs for patients, students and staff across the hospital.
Abstract:
People with eating disorders adhere to rigid rules that maintain their disorder. During recovery, these rules fade and new rules are developed. Unfortunately, the rest of the world doesn’t nurture the same recovery focused rules so recovery can be a minefield for many people. Our clients with eating disorders are surrounded by a world that nurtures unrelenting standards and unhealthy relationships to food, weight and shape Popular western culture objectifies women and encourages scrutiny, manipulation and transformation of bodies. Social media, television and sexist advertising impact negatively on body satisfaction, self-esteem (Bardone-Cone & Cass, 2007; Tiggemann & Slater, 2013), the perception of heaviness in the body and lowered self-worth (Bardone-Cone & Cass, 2007), and influence eating behaviour (Smith, Hames, & Joiner Jr., 2013). Many women internalise the ‘thin ideal’ (Thompson & Stice, 2001), take a hyper-critical observer perspective of their body (Fredrickson & Roberts, 1997) which then influences body-hatred. Gendered cultural context plays a role in the development and maintenance of eating disorders. The aim of this presentation is to highlight the different rules that people in recovery from eating disorders have noticed they need to live by when compared to the rest of the world. Sonja will present some recovery oriented rules that her clients have developed, some that research recommends and others that she has observed in her clinical experience as being essential to recovery and maintaining a recovery focused view. Recommendations for clients with eating disorders, their families and friends as well as clinicians working in this field will be discussed.
Andrea Pousada
Saint Louis University, Spain
Title: Applied neuroscience using neurofeedback in the treatment of mental health conditions
Time : 14:25-14:55

Biography:
Dr. Andrea Pousada is a Professor at Saint Louis University (Madrid Campus). She has a B.S. and M.S. in Clinical Psychology and a Ph.D. in Neuroscience. Her postdoctoral research at Harvard University focused on fMRI, biomarkers and cognitive endophenotypes in patients in high-risk for psychosis and bipolar disorder as well as the use of transcranial magnetic stimulation (TMS) as a therapeutic alternative for negative symptoms in schizophrenia. Nowadays she combines her work in the academic field with private practice as a clinical psychologist/neuropsychologist and applying neuroscience techniques to improve different health conditions as well a neuroscience consultant in other fields.
Abstract:
Applied neuroscience is an emerging field that aim to use the latest findings from brain science into clinical interventions to improve human functioning. Neurofeedback is one of the techniques from the neuroscience field that has been proven to be effective when applied in the clinical field in many conditions such as ADHD, ASD, depression, anxiety, autism among others. Neurofeedback is a non-invasive technique based on electroencephalography (EEG) that registers brain activity in order to provide the patient with a feedback that will help patients to regulate their brain activity and, consequently, improving brain functioning. Therefore, in recent years, research has shown that neurofeedback is a powerful therapeutic technique to improve health conditions and cognitive functions through neuroplasticity, recovering connections between neurons or creating new neural pathways. At the end of the talk, a clinical case of autism will be used to explain the effectiveness of the technique by facilitating improvement in areas of abnormal connectivity and stabilizing brain activity which triggers a reduction of symptoms and positive behavioral changes, increasing the quality of the patient diagnosed with ASD and the relatives. Some of the improvements that can be achieved using neurofeedback in patients diagnosed with autism are related to more distinctiveness in speech, more stable mood, increase in tolerating changes in the environment and physical contact, decreased loud outbursts, social communication as well as a significant improvement in terms of cognitive functions.
Neeta Sinha
Pandit Deendayal Petroleum University, India
Title: Psycho-Social analysis of challenges facing India’s smart cities
Time : 14:55-15:25

Biography:
Neeta Sinha is a Behavioural Psychologist, Academician and Corporate Trainer. She hold Ph.D. in the interdisciplinary area of Psychology and Management. Has more than 12 years of Corporate experience and 13+ years of teaching experience. She has published and presented more than 25 papers in reputed journals and is the Managing Editor of the journal ‘Liberal Studies’. She is on the editorial board of several journals and also on the advisory board in many universities. Dr.Sinha is also the Chairperson, PhD. Program at PDPU.
Abstract:
Smart city concept entails four main system components which includes:
Smart technology (including ICT)
Smart innovation
Smart system
Smart people
In the Indian context why emphasis leans towards the first three which are variously defined and discussed in terms of the intervention, there seems to be an absence of clarity in terms of smart people. Since the word smart in the broader sense of the term refers to application of certain kind of intelligence in finding solutions to the problems at people’s level it also becomes a training and behavioral issue. To make it simpler, what is meant here is that using smart technology and innovation efficiently would inevitable require smart behaviour as well.
In India, which is the case in point here, due to its enormous socio cultural and economic heterogeneity the people still lag the refinement in public behavior more particularly when it comes to meeting the basic expectation of sanitation, compliance to traffic rules, ecological awareness among other.
Since there is a lack of bench marking in the minimum level of social behaviour even the most efficient technologies and systems often fail to deliver the desired result. Eg. Open defecation, urinating in public places, spitting in public buildings, throwing remains of gutka and pan masalas in wash basins and urinals, general disobedience of traffic rules such as jumping signals, risky driving, chaotic parking are some of the basic issues which are rampant across India. These problems are not just related to infrastructure deficits as such but also with psycho social behaviour for which little efforts towards its improvement have been attempted. Since technology alone cannot find all the answers, it can only be used to increase the efficiency of performance, a major change is actually required at the psycho-social behavioral level. It implies an operant conditioning (Skinner 1938) of sorts which includes both reward and reprimand.
This paper will try to deal with the psycho-social aspect of the urban dwellers in India to propose the required benchmarking for smart people for smart cities.
Yi Lei
Shenzhen University, Republic of China
Title: How do the hierarchical levels of premises affect category-based induction: Diverging effects from the P300 and N400
Time : 15:45-16:15

Biography:
Yi Lei, Associate Professor of Department of Psychology and Sociologyat Shenzhen University, received her Ph.D. from Southwest University of Developmental and Educational Psychology (2007). Her main researches explore the interaction between semantic relationship and emotion. So far, she has published 31 papers in international SCI/SSCI journals such as Neuropsychologia, Biological psychology, Neuroimage, Scientific Reports, Experimental brain research , International Journal of Psychophysiology, as well as national core journals such as Acta Psychologica Sinica, Psychological Development and Education, Advances in Psychological Science, Psychological Science. She also won the Excellent Doctor Degree and Excellent Doctorial Dissertation Awards of Southwest University.
Abstract:
Although a number of studies have explored the time course of category-based induction, little is known about how the hierarchical levels (superordinate, basic, subordinate) of premises affect category-based induction. The EEG data were recorded when nineteen healthy human participants were performing a simplifed category-based induction task. The ERP results showed that: in the subordinate conclusion condition, the basic premise elicited a larger N400, versus the superordinate premise; in the basic conclusion condition, the superordinate premise elicited a larger P300 relative to both the basic premise and subordinate premise; in the superordinate conclusion condition, however, no difference was found between different premises. Furthermore, the process that reasoning from a higher level to a lower level evoked a larger P300, compared to it did in the reverse direction. The divergent evidence suggested that category-based induction at superordinate, basic, and subordinate levels might be affected by various factors, such as abstract level, direction, and distance between premise and conclusion, which yielded new insights into the neural underpinnings of category-based induction with different inductive strengths.
Chao Wang
Shenzhen University, Republic of China
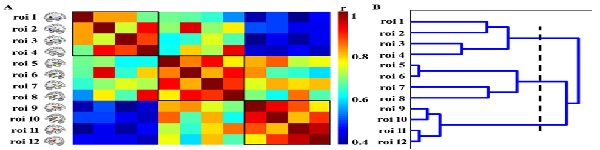
Title: Disrupted functional connectivity patterns of the insula subregions in durg-free major depressive disorder
Time : 16:15-16:45

Biography:
Chao Wang has completed her PhD in 2015 from University of Electronic Science and Technology of China. She is the assistant professor of Shenzhen University. The research areas that her works on include imaging genomics, brain network analysis, and their applications in the individual differences of cognitive function and risk for psychiatric disorders. She has publised four papers as first author in reputed journals, such as the Journal of Neuroscience,Neuroscience and journal affective of disorders. Dr. Wang is undertaking two research projects supported by the National Natural Science Foundation of China (NSFC) and Shenzhen University.
Abstract:
Major depressive disorder (MDD) is characterized by impairments in emotional and cognitive functions. Emerging studies have shown that cognition and emotion interact by reaching identical brain regions, and the insula is one such region with functional and structural heterogeneity. Although previous literatures have shown the role of insula in MDD,it remains unclear whether the insular subregions show differential change patterns in MDD. Using the resting-state fMRI data in a group of 23 drug-free MDD patients and 34 healthy controls (HCs), we investigated whether the abnormal connectivity patterns of insular sub-regions or any behavioural correlates can be detected in MDD. Further hierarchical cluster analysis was used to identify the functional connectivity-clustering patterns of insular sub-regions. Compared with HCs, the MDD exhibited higher connectivities between dorsal agranular insula and inferior parietal lobule and between ventral dysgranular and granular insula and thalamus/habehula, and lower connectivity of hypergranular insula to subgenual anterior cingulate cortex (Figure 1). Moreover, the three subregions with significant group differences were in three separate functional systems along anterior-to-posteior gradient (Figure 2). The anterior and middle insula showed positive correlation with depressive severity, while the posterior insular was to the contrary (Figure 1). These findings provided evidences for the MDD-related effects in functional connectivity patterns of insular subregions, and revealed that the subregions might be involved in different neural circuits associated with the contrary impacts on the depressive symptoms.
Figure 1:
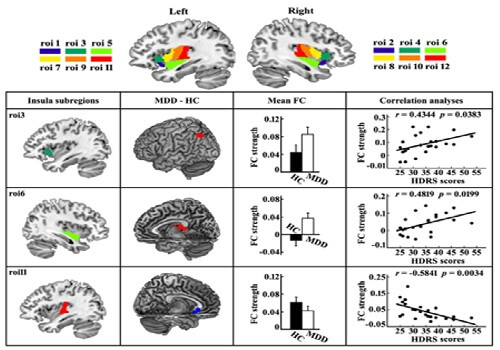
Figure 2:
A Vishal
Nizamabad Medical College, India
Title: Outcomes in patients with first episode schizophrenia treated with long-acting antipsychotic injections
Time : 16:45-17:15

Biography:
A Vishal has completed his MD in Psychiatry from NTR University of Health Sciences, Vijayawada. Now, he is working as Assistant Professor of Psychiatry at Government Medical College, Nizamabad, Telangana, India.
Abstract:
Background: Noncompliance is a major problem for patients with first episode schizophrenia. Long-acting injectable antipsychotics (LAI APs) should offer better efficacy and tolerability compared to oral antipsychotics due to improved adherence and more stable pharmacokinetics. LAI APs have proved the effectiveness in first episode schizophrenia because they assure stable blood levels leading to a reduction of the risk of relapse.
Objectives: The objective is to compare the clinical efficacy of the long-acting injectable antipsychotics with the oral antipsychotics in the first episode of schizophrenia.
Methods: Parameters were assessed at baseline and at 3 month intervals for 2 years in patients initiated on long-acting injection (LAI) (n=673) or a new oral antipsychotics (AP) (n=139 on risperidone and olanzapine) at Nizamabad. Hospitalization prior to therapy was assessed by a retrospective chart review.
Results: At two years treatment retention and reduction in Clinical Global Impression Severity, scores were significantly higher with LAI. Compared to the pre-switch period, LAI Aps patients had greater reductions in the number of hospitalizations at two years than oral AP patients.
Conclusions: This study showed that, compared to oral antipsychotics, LAI APs were associated with better treatment retention, greater improvement in clinical symptoms and functioning and greater reduction in hospital stays and days at hospital in patients with first episode schizophrenia.
Annamarie Paulsen
Rockdale Psychiatric Associates, USA
Title: Successful Outpatient Treatment of Opiate Addiction

Biography:
Annamarie Paulsen MD is a Board Certified in Child, Adolescent and Adult Psychiatrist and former nurse with over thirty five years working in a multidisciplinary psychiatric setting in the US. She is a Medical Director in Rockdale Psychiatric Associates Conyers, Georgia USA. She did her Bachelors of Nursing in Medical College of Georgia. In Emory University she completed her Masters in Nursing. In University Of Iowa she accomplished her Masters in Preventive Medicine and Psychiatric Epidemiology. She completed her Doctor of Medicine in Morehouse School of Medicine.
Abstract:
Looking forward to our "Sublocade Launch” AND looking back on over five years of outpatient treatment of opiate addiction in a suburban private USA psychiatric practice using Suboxone or generic buprenorphine. The presenters will give a detailed description of their experience using buprenorphine and naltrexone combination medications to treat opiate addiction. We will cover our successes and our struggles to treat clients who are opiate-dependent highlighting best practice methodologies.
The attendees will be "brought into our clinic" to better understand how to liaison with therapists, community resources and and family and friends. We will describe in detail our treatment protocol and our emphasis on 12- step principles and therapy techniques including DBT and Emotional Freedom Tapping. We will give real-life examples of these treatment modalities reinforce a growing sense of self-love, compassion and self- forgiveness. We will also review the use of these medications in clients with medical conditions and at varying stages of life. We will also highlight our early clinical experience with Sublocade, the new monthly injection form of buprenorphine. This new delivery system will eliminate some of the difficulties associated with the prescription of oral agents. We will present the management of our clients using this new delivery system.
Lehel Simon
Entactex Pharma Research Project, Hungary
Title: Levente Szilágyi: An outlook on the genetics of autisms and analogue conditions from a cognitive science perspective and the possibility of a personalized polymer amine therapy
Biography:
Lehel Simon graduated as a Master of Philosophy, the theme of my PhD Dissertation is Biopsychology. Lately I have been engaged with leading a PET - MRI hypothalamus research in the Entactex Pharma Research Project. Our Research Team has a patent for a central vasopressin receptor - antagonist, which can be a medicine in negativistic syndromes (like oxytocin nasal spray, but directly, not only in peripherial infusion like oxytocin) for example in autism spectrum disorder. Moreover it is in interaction with GnRH, oxytocin, dopamine, prolactin, so it can be applied in cases of female anorgasmia, too. The research is being conducted in several countries all over the world.
Abstract:
Autisms have been examined from many aspects: as clinical description, by means of the nowadays popular cognitive psychology, from a brain anatomy aspect (see corpus callosum and hypothalamus lesion), as the subject of genetics (X - fragility) and from the gender aspect (see Asperger syndrome: “male brain disorder”). But scientist so far failed to even try to combine these models.
Clinical description can now be proven by cognitive psychology (see “Read the Mind” -tests) – this is a matter of fact. For example corpus callosum-lesion can be explained by this, and X-fragility can be explained by the gender relevancies of the aforementioned and so on.
A unified biochemical model has not been developed yet while the scientific media is loud about the oxytocin, secretin, ondansetron and naltrexone experiments. What are their common aspects in the nucleus suprachiasmaticus of the hypophysis? It has been suspected that this is where the resolution lies but we have not had a biochemical model.
The ultimate question in our study is as follows. Can a stable and healthy state of the hypothalamic balance be established in the nucleus suprachiasmaticus? We examine every brain research aspects of this from gender to neuro-biochemistry to make a futuristic suggestion which can be easily accomplished taking the modern drug technology into consideration by testing the applicableness of peptide operator polymer amines – focusing on the neuropeptides of hypothalamus.
Robert P. Franks
Judge Baker Children’s Center/Harvard University, USA
Title: Improving the Quality of Behavioral Healthcare for Children and Adolescents
Biography:
Dr. Robert P. Franks is president and chief executive officer of Judge Baker Children's Center in Boston, MA, USA. Dr. Franks, a leader in the implementation and dissemination of evidence-based practices in children’s mental health, holds a master’s degree from George Washington University and a Ph.D. from Boston College. He completed his clinical training and doctoral fellowship in child psychology at the Yale University Child Study Center. Dr. Franks has provided direct service, consultation and technical assistance to programs and initiatives in early childhood, mental health, child welfare, education and juvenile justice at the local, state and national levels. Dr. Franks is a senior lecturer in Psychology in the Department of Psychiatry at Harvard Medical School.
Abstract:
Statement of the Problem: Despite major advances in understanding what works best in the treatment of a wide range of behavioral health problems in children and adolescents, a significant gap remains between research and practice. To address this gap, intermediary organizations have been developed to work with treatment developers and community based providers to implement best practice models of care and train practitioners to deliver high quality services with good outcomes. This presentation will provide an overview of this methodology and a case study of how behavioral health services were improved within a statewide system of care.
Methodology & Theoretical Orientation: This presentation will provide an overview of the roles and functions of an intermediary organization working to improve behavioral health services in a statewide system, as well as the implementation framework used to train and disseminate an evidence-based practice, the Modular Approach for Treatment of Children with Anxiety, Depression, Trauma and Conduct (MATCH). A brief overview of the MATCH model will be presented followed by a discussion of implementation strategies and system wide outcomes resulting in improved quality of care.
Conclusion & Significance: As the need for effective services for children and adolescents grows, it is vital that we explore effective mechanisms to train providers in evidence-based models to improve the quality of care. This presentation will demonstrate an effective strategy that has been used to train behavioral health providers impacting thousands of families. This model can be replicated in other settings around the world.
Sue Cornbluth
International Parenting Expert, USA
Title: Children, trauma and self Esteem : The strategies professionals and parent must learn to lead traumatized children to success
Biography:
Dr. Sue Cornbluth is a internationally recognized and certified parenting expert in high conflict parenting situations. In 2013, Dr. Sue created the consulting firm Parenting Beyond Trauma, LLC which helps parents move through and beyond their high conflict divorces. Dr. Sue earned her reputation as a leading expert in child abuse and victims' rights during the Jerry Sandusky trial. She is a regular mental health contributor for an array of networks and television shows such as NBC, FOX and CBS. Currently she is the host of her own radio show called, "The Dr. Sue Show" on http://www.streamcity.org/dr-sue-show. She has contributed to several national publications as well. Her new best-selling book, “Building Self-esteem In Children And Teens Who Are Adopted or Fostered” is available now.
Dr. Sue's passion is to make a difference in the lives of traumatized children by educating parents and professionals about how to help children succeed in life. She travels throughout the country speaking at conferences about her work.
Recently, Dr. Sue was named one of the most "Distinctive Women" in the country by Women's Distinctive Business Magazine. Dr. Sue holds a doctoral degree in Clinical Psychology and was a former psychology professor at Temple University. She lives outside of Philadelphia, PA with her husband and two children.
Abstract:
There are millions of children all across this world who suffer or have suffered some form of child abuse; whether that be physical, sexual, neglect or emotional. Research tells us that due to this abuse, 80 % of these children can suffer attachment disorders as they grow older. (Leavy & Orleans 2014). This means that due to abusive relationships, children without proper help to heal will most likely end up in unhealthy adult relationships. More importantly, children lacking secure attachments are at a high risk of growing up to be parents who are incapable of establishing a secure connection with their children. Healthy parent child relationships are the cornerstone of strong developmental growth. When neglect or emotional and physical abuse occurs, the parent and child relationship can become very complicated and at times even severed.
In this keynote speech Dr. Sue talks about inspiring abused and neglected children to reach their full potential by helping them to see that they are more than the abuse they have suffered. Dr. Sue shares her personal story of helping a 16 year old abused foster child overcome low self esteem , physical abuse and self hatred to become a graduate of college and a successful mother. Fourteen years later, this young woman wrote the forward for Dr. Sue's new bestselling book, "Building-Self esteem in Children and Teens Who Are Adopted or Fostered." Dr. Sue also talks about how professionals are the "catalyst" to helping abused and neglected children move to a successful place in their lives in her speech. She shares her 3 Tier- Empowerment-Model that was based on her ground breaking research with abused children which is used by professionals worldwide to help abused and neglected children raise their self esteem.
Biography:
Deanna Mulvihill has her expertise in evaluation and passion in improving the health and wellbeing. Her open and contextual evaluation model based on responsive constructivists creates new pathways for improving healthcare. She has built this model after years of experience in research, evaluation, teaching and administration both in hospital and education institutions. The foundation is based on fourth generation evaluation (Guba& Lincoln, 1989) which is a methodology that utilizes the previous generations of evaluation: measurement, description and judgment. It allows for value-pluralism. This approach is responsive to all stakeholders and has a different way of focusing.
Abstract:
Statement of the Problem: Women who have experienced intimate partnerviolence (IPV) are at greater risk for physical and mental health problems including posttraumatic stress disorder (PTSD) and alcohol dependency. On their own IPV, PTSD and alcohol dependency result in significant personal, social and economic cost and the impact of all three may compound these costs. Researchers have reported that women with these experiences are more difficult to treat; many do not access treatment and those who do, frequently do not stay because of difficulty maintaining helping relationships. However, these women’s perspective has not been previously studied. The purpose of this study is to describe the experience of seeking help for alcohol dependency by women with PTSD and a history of IPV in the context in which it occurs.
Methodology & Theoretical Orientation: An inter subjective ethnographic study using hermeneutic dialogue was utilized during participant observation, in- depth interviews and focus groups. An ecological framework was utilized to focus on the interaction between the counselors and the staff to understand this relationships and the context in which it occurs. Findings: The women in this study were very active help seekers. They encountered many gaps in continuity of care including discharge because of relapse. Although the treatment center was a warm, healing and spiritual place, the women left the center without treatment for their trauma needs and many without any referral to address these outstanding issues. Conclusion & Significance: Women with alcohol dependence and PTSD with a history of IPV want help however the health and social services do not always recognize their calls for help or their symptoms of distress. Recommendations are made for treatment centers to become trauma- informed that would help this recognition.
Mario E. Martinez
PsyD Nashville, USA
Title: The Mind body self: How longevity is culturally learned and the causes of health are inherited
Biography:
Mario Martinez is a US clinical neuropsychologist who specializes in how cultural beliefs affect health and longevity. He proposes, based on credible research evidence, that longevity is learned and the causes of health are inherited. He has studied healthy centenarians (100 years or older) worldwide and found that only 20% to 25% can be attributed to genetics the rest is related to how they live and the cultural beliefs they share. Dr. Martinez is the author of the bestselling books The MindBody Code: How to Change the Beliefs that Limit Your Health, Longevity, and Success and The MindBody Self: How Longevity is Culturally Learned and the Causes of Health Are Inherited, that teach his theory and practice of bio cognitive science to professionals and the general public. In addition to longevity, he also proposes how our immune system is not just a protector. Instead, it responds to the cultural premises we learn to perceive the world.
Abstract:
We know that the mind influences the body, but what seems to be ignored in the life sciences is what influences the mind. I propose why culture is what influences the mind by creating a context for the communication. Based on my ethnography work with healthy centenarians worldwide, I describe how cultural beliefs are more powerful than our genetic endowment, and how growing older is mostly the passing of time, whereas aging is what we do with our time based on the beliefs we assimilate from our cultures. Rather than being genetically sentenced with family illnesses, we have the capacity to change how our genes express disease as well as the causes of health, based on how our brain learns to culturally perceive the world. My theory and practice of mind body science is based on research that investigates the healthy brains, the exalted emotions (compassion, empathy, love), and the elevated cognitions (honor, admiration, cooperation). As Homo sapiens, our immune system has 150,000 years of accumulated wisdom that has allowed it to evolve from a protector against pathogens to an intelligent interpreter that confirms the cultural beliefs that we choose to engage. Bio cognitive science studies the outliers of the normal curve. Conventional science studies averages at the expense of individual differences. Researching outliers provides valuable individual characteristics missed on group research. These individual characteristics help clarify exceptions in prognosis of terminal illnesses, spontaneous remissions, individual components of longevity, and causality in cultural contexts.
Quynh-Anh Nguyen
Monash University, Australia
Title: Validation of the trait emotional intelligence questionnaire – Adolescent short form (TEIQue-ASF) among adolescents in Vietnam
Biography:
Abstract:
Statement of the Problem: — Trait Emotional Intelligence is the knowledge, beliefs, and attitudes an individual has about their own and other people’s emotions. It is believed that trait emotional intelligence is a component of personality. Petrides’ Trait Emotional Intelligence Questionnaire (TEIQue) is well regarded and well-established, with validation data about its functioning among adults from many countries. However, there is little data yet about its use among Asian populations, including adolescents. The aims were to translate and culturally verify the Trait Emotional Intelligence Adolescent Short Form (TEIQue-ASF) and investigate content validity, construct validity, and reliability among adolescents attending high schools in Vietnam. Methodology & Theoretical Orientation: Content of the TEIQue-ASF was translated (English to Vietnamese) and back-translated (Vietnamese to English) in consultation with bilingual and bicultural health researchers and pilot tested among 51 potential respondents. Phraseology and wording were then adjusted and the final version is named the VN-TEIQue-ASF. The VN-TEIQue-ASF’s properties were investigated in a cross-sectional self-report survey among high school students in Central Vietnam. Findings: In total 1,546 / 1,573 (98.3%) eligible students from nine high schools in rural, urban, and coastline areas completed the survey. Explanatory Factor Analysis yielded a four-factor solution, including some with facets that loaded differently compared to the original version: Well-being, Emotion in Relationships, Emotion Self-management, and Emotion Sensitivity. The Cronbach’s alpha of the global score for the VN-TEIQue-ASF was .77. The VN-TEIQue-ASF is comprehensible and has good content and construct validity and reliability among adolescents in Vietnam. The factor structure is only partly replicated the original version. Conclusion & Significance: The VN-TEIQue-ASF is recommended for use in school or community surveys and professional study in education, psychology, and public health to investigate the trait emotional intelligence of adolescents in Vietnam.
Zelda G Knight
University of Johannesburg, RSA
Title: “If I leave home, who will take care of mum?†Intergenerational transmission of parental trauma through projective identification
Biography:
Zelda Knight is a PhD graduate of Rhodes University, South Africa, and an experienced practising psychotherapist, as well as a Professor of Psychology at the University of Johannesburg. She has been lecturing for many years and has a substantial publication record with works published in international journals and academic books. She is an NRF Rated Scientist in her country which means that she is recognised by peers as an expert within the field of psychotherapy. She has presented numerous papers at international conferences worldwide, including being a keynote speaker on several occasions. She is currently the Vice President of the World Council for Psychotherapy (African Chapter), and on the Editorial Board of several academic journals in psychology and psychotherapy. She is involved in the psychotherapy training of Clinical and Counselling Master’s students at the University.
Abstract:
Using the construct of projective identification and integrating it with the body of literature on intergenerational transmission of unsymbolized parental trauma, I describe the case of an adult daughter that illustrates intergenerational transmission of unsymbolized parental trauma. It is suggested that the daughter has unconsciously identified with the disavowed feelings of anxiety projected into her by her mother. The daughter’s projective identification of her mother’s unresolved past traumas prevent her from leaving the parental home for the first time, despite being 35 years old. In turn, it is thought that the mother’s unconscious grasping onto her daughter is an attempt to avoid the confrontation of her own unprocessed fears implanted into her by her own mother, thus linking three generations of disavowal. As a way of extending the exiting theory, it is proposed that when there is long-term and inexplicable experiences of anxiety that coalesces around the intergenerational transmission of parental trauma, the term ‘intergenerational transmission of traumatic anxiety’ can be used to describe it.
Richard Chambers
Monash University, Australia
Title: Creating a mindful university to boost mental health and performance
Biography:
Dr Richard Chambers is a clinical psychologist and internationally-recognised expert in mindfulness. He is leading a university-wide mindfulness initiative at Monash University, as outlined in his 2017 TEDx talk. Richard regularly provides mindfulness training to a growing number of businesses, educational institutions and community organisations. He has been teaching mindfulness since 1999 and regularly provides lectures and workshops around Australia and internationally.
Richard helped develop Smiling Mind, a free mindfulness app with over 2.5 million downloads, and the Mindfulness for Wellbeing & Peak Performance free online course which has had 230,000 users and was ranked within the Top 50 online course of all time by Class Central. He has published three books, Mindful Learning, Mindful Relationships and Mindful Origami. He features regularly in mainstream media and is actively involved in research studies at a number of universities around Australia.
Abstract:
University students are facing unprecedented academic and social pressures. Combined with the fact that most mental health disorders emerge in adolescence and young adulthood, research has found elevated levels of stress, anxiety and depression amongst tertiary students, often impacting academic performance. Mindfulness has been shown to increase resilience, improve mental health and boost cognitive/study performance. It also increases self-awareness and interpersonal functioning. Monash University in Melbourne, Australia is piloting a novel university-wide mindfulness initiative, embedding mindfulness in the core curriculum for students, offering optional programs for staff and pioneering online delivery methods. As far as we know, we are the only university in the world attempting to deliver mindfulness on such a scale. Our research has found our programs and curricula are generally well received and lead to significant improvements in both mental health and work/study engagement. Our programs also contributed to Monash winning the World Health Organisation’s “World’s Healthiest Workplace” award in 2017. This keynote presentation outlines the underling rationale, the innovative nature of our approach and the results of our formal evaluations.
Meng Zi Jie Aaron
Ministry of Health Holdings, Singapore
Title: Olfactory reference syndrome- A case report
Biography:
Meng Zi Jie Aaron, MBBS (Singapore), MRCPsych (UK) is a graduate of Yong Loo Lin School of Medicine from the National University of Singapore. He is currently a Senior Resident of the local Psychiatry residency programme and is in his final year of training at Ng Teng Fong General Hospital. He has undergone rotations in most fields of Psychiatry, including adult general psychiatry, child and adolescent psychiatry, psychogeriatric, addiction medicine, consultation and liason psychiatry and forensic psychiatry.
Abstract:
Background: Olfactory reference syndrome (ORS) is an interesting psychiatric condition which is characterised by a preoccupation that one emits body odour, which is not perceived by others. While anecdotally described as a discrete condition, its phenomenological overlap between anxiety and psychotic disorders poses a challenge in diagnostic classification.
We present a case of a 19 year old Chinese Male who was referred through his gastroenterologist for having a fixed persistent belief of having an offensive body odour, which seemingly worsened after his mother had passed away. He was found to have significant anxiety and coped with safety behaviours which had become maladaptive with time. His excessive worries were also associated with psychotic symptoms of referential delusions and olfactory hallucinations related to flatulence.
As in our case, the clinical picture of ORS may cross both anxiety and psychotic symptoms and warrants further review in the latest diagnostic classification manual.
- Psychiatric Nursing | Neuro Cognitive Disorder | Couple Therapy for Psychological Disorders | Psychotherapy | Dialectical Behavior Therapy | Behavioral Therapy | Cognitive Behavioral Therapy | Emotion Regulation Therapy